Contents
-
When Are Antibiotics Needed?
-
Choosing the Right Antibiotic
-
Risks and Benefits
Antibiotics: A Lifeline for COPD Exacerbations?
Antibiotics: A Lifeline for COPD Exacerbations?
The Big Picture
Antibiotics can be a game-changer during COPD flare-ups, but when are they really necessary? Let's explore how they help and when they're needed.
Contents
-
When Are Antibiotics Needed?
-
Choosing the Right Antibiotic
-
Risks and Benefits
When Are Antibiotics Needed?
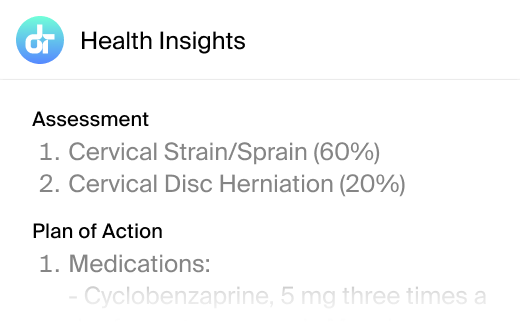
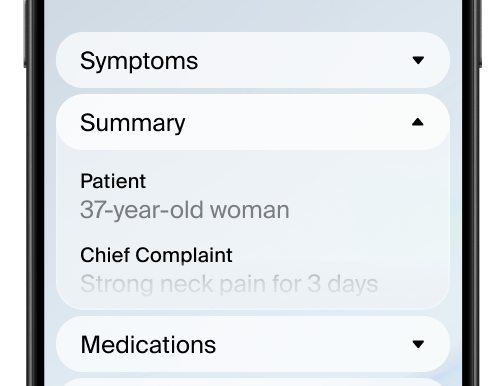
Antibiotics are typically used when a bacterial infection is suspected during a COPD exacerbation. Key signs include increased difficulty breathing, more mucus, and a change in mucus color. Severe cases requiring hospitalization may also call for antibiotic treatment.
Choosing the Right Antibiotic
Choosing the right antibiotic depends on the severity of the exacerbation and any previous antibiotic use. Common options include azithromycin and amoxicillin-clavulanate, which target the most likely bacteria causing the infection.
Risks and Benefits
While antibiotics can reduce recovery times, they also carry risks like antibiotic resistance. It's crucial to balance these benefits and risks, especially in mild cases where antibiotics may not be needed.
FAQs
When should antibiotics be used for COPD?
They're used for suspected bacterial infections during severe exacerbations.
Which antibiotics are commonly used?
Azithromycin and amoxicillin-clavulanate are common choices.
What are the risks of using antibiotics?
They can lead to antibiotic resistance and other side effects.
Key Takeaways
Antibiotics are crucial for certain COPD exacerbations but must be used wisely.
Additional References
-
National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease (acute exacerbation): antimicrobial prescribing. July 2018.
-
Rothberg MB, Pekow PS, Lahti M, et al. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA 2010; 303:2035.
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.