Heparin in Pregnancy: Balancing Mom and Baby's Health
Heparin in Pregnancy: Balancing Mom and Baby's Health
A Delicate Balance
Pregnancy increases the risk of blood clots, but many blood thinners can harm the developing baby. Heparin offers a unique solution, providing protection for mom without crossing the placenta to affect the fetus.
Contents
- Why Heparin in Pregnancy?
- When is it Recommended?
- Dosing and Monitoring
- Considerations for Delivery
Why Heparin in Pregnancy?
During pregnancy, a woman's blood naturally becomes more prone to clotting. This protects against excessive bleeding during childbirth, but it also increases the risk of dangerous blood clots. Some women, especially those with certain health conditions, need extra protection. Heparin, particularly low molecular weight heparin (LMWH), is the preferred blood thinner because it doesn't cross the placenta to affect the baby.
When is it Recommended?
Heparin might be prescribed if you have a history of blood clots, certain heart conditions, or inherited clotting disorders. It's also used to prevent miscarriage in women with antiphospholipid syndrome. The decision to use heparin is always individualized, weighing the potential benefits against any risks.

Dosing and Monitoring
LMWH is usually given as a daily injection under the skin. The dose may need to be adjusted as your pregnancy progresses and your weight changes. While routine monitoring isn't always necessary, your doctor will keep a close eye on your health. They may check your platelet count and, in some cases, measure heparin levels in your blood.
Considerations for Delivery
As you near your due date, your doctor will create a plan for managing your heparin around delivery. You'll usually stop heparin injections 24 hours before a planned delivery or when labor starts. This reduces the risk of excessive bleeding. Heparin can often be restarted shortly after delivery if needed.
FAQs
Is heparin safe for breastfeeding?
Yes, it doesn't pass into breast milk in significant amounts.
Will I need heparin for my whole pregnancy?
It depends on your individual risk factors and reason for treatment.
Can heparin prevent miscarriage?
In certain conditions like antiphospholipid syndrome, it may help.
Are there alternatives to injections?
Unfortunately, oral blood thinners aren't safe in pregnancy.
Will heparin affect my baby's development?
No, heparin doesn't cross the placenta to reach the baby.
A Valuable Tool
While not needed for all pregnancies, heparin offers crucial protection for high-risk moms without compromising fetal safety.
Additional References
- Bates SM, et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e691S-e736S.
- Fogerty AE. Challenges of Anticoagulation Therapy in Pregnancy. Curr Treat Options Cardiovasc Med. 2017;19(10):76.
- Schaefer C, et al. Drugs During Pregnancy and Lactation (Third Edition), 2015. Chapter 2.6 - Anticoagulants and Thrombolytics.
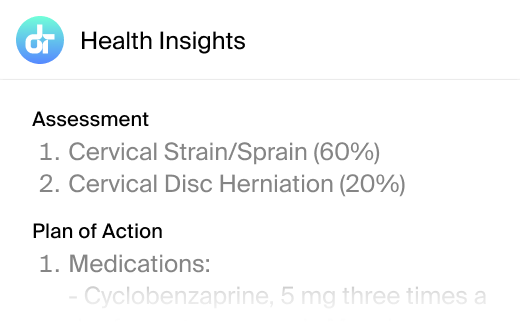
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.