Medical Guidelines for Managing Infective Endocarditis
Medical Guidelines for Managing Infective Endocarditis
Guiding Principles
Following medical guidelines can help manage and treat infective endocarditis effectively.
Contents
- Diagnosis and Monitoring
- Treatment Options
- Preventive Measures
- Patient Education
Diagnosis and Monitoring
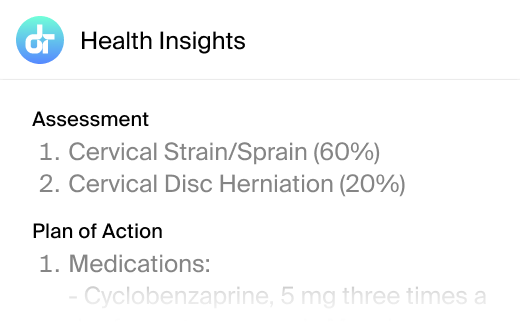
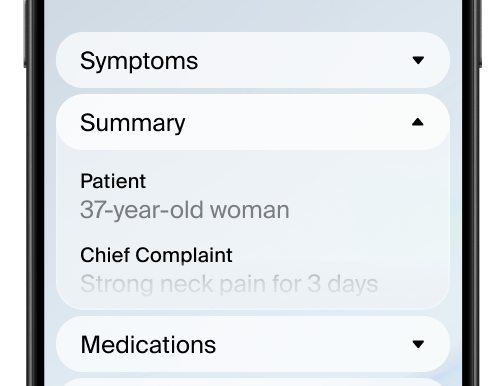
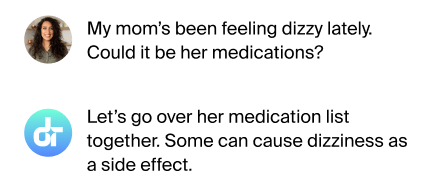
Accurate diagnosis is crucial for effective treatment of infective endocarditis. It involves blood cultures and echocardiography to detect the presence of bacteria and assess heart valve damage. Regular monitoring is essential to track the progress of treatment and adjust medications as needed.
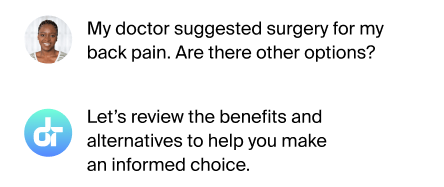
Treatment Options
Treatment typically involves long-term antibiotic therapy tailored to the specific bacteria identified. In severe cases, surgical intervention may be necessary to repair or replace damaged heart valves. Early and appropriate treatment can significantly improve outcomes.

Preventive Measures
Medical guidelines recommend preventive measures such as maintaining good dental hygiene and avoiding high-risk behaviors like drug use with needles. For certain patients, antibiotics before medical or dental procedures are advised to prevent infection.
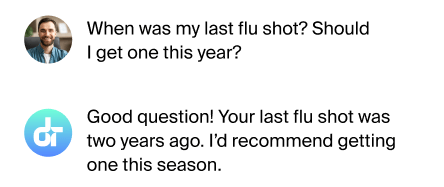
Patient Education
Educating patients about the risk factors and symptoms of infective endocarditis is vital. Understanding when to seek medical help can prevent serious complications and improve overall prognosis.
FAQs
How is infective endocarditis diagnosed?
Through blood cultures and echocardiography to detect bacteria and valve damage.
What treatments are available?
Long-term antibiotics and possibly surgery for severe cases.
Are preventive measures recommended?
Yes, such as good dental hygiene and antibiotics for high-risk patients.
Why is patient education important?
It helps patients recognize symptoms and seek timely medical help.
Is regular monitoring needed?
Yes, to ensure treatment effectiveness and adjust as necessary.
Final Thoughts
Following guidelines can make a significant difference in managing infective endocarditis.
Additional References
- Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2007; 116:1736.
- Fowler VG Jr, Miro JM, Hoen B, et al. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA 2005; 293:3012.
- Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009; 169:463.
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.