Treating Chronic Mesenteric Ischemia: Clearing the Gut's Traffic Jam
Treating Chronic Mesenteric Ischemia: Clearing the Gut's Traffic Jam
Restoring the Flow
Chronic mesenteric ischemia occurs when blood flow to the intestines is reduced. This article explores the various treatment options available to restore proper circulation and relieve symptoms.
Contents
- Endovascular Treatment: The Minimally Invasive Approach
- Open Surgery: When More is Needed
- Hybrid Procedures: The Best of Both Worlds
- Medical Management: Supporting Overall Health
Endovascular Treatment: The Minimally Invasive Approach
Endovascular procedures are often the first-line treatment for chronic mesenteric ischemia. These minimally invasive techniques include angioplasty (balloon inflation to widen arteries) and stenting (placing a mesh tube to keep arteries open). It's like using a tiny plumber's snake to clear a clogged pipe. These procedures have a quicker recovery time and lower initial risks compared to open surgery.
Open Surgery: When More is Needed
For some patients, open surgery may be necessary. This typically involves bypass surgery, where a new blood vessel is created to route blood around the blockage. Think of it as building a detour around a traffic jam. While more invasive, open surgery often provides more durable results, especially in younger, healthier patients.

Hybrid Procedures: The Best of Both Worlds
Hybrid procedures combine elements of both endovascular and open surgical techniques. For example, retrograde open mesenteric stenting (ROMS) involves surgically accessing an artery and then placing a stent. This approach can be particularly useful in complex cases or when treating acute symptoms.
Medical Management: Supporting Overall Health
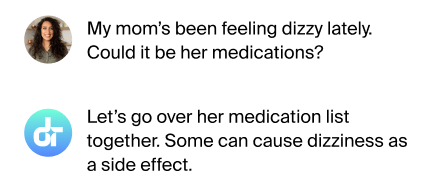
In addition to revascularization procedures, medical management plays a crucial role. This includes medications to prevent blood clots, control blood pressure, and manage cholesterol. Lifestyle changes like quitting smoking and improving diet are also important. Think of this as routine maintenance for your body's highway system.
FAQs
Which treatment is best for chronic mesenteric ischemia?
The best treatment varies by patient; endovascular procedures are often tried first.
How long is the recovery after treatment?
Recovery ranges from days for endovascular procedures to weeks for open surgery.
Are these treatments permanent?
While effective, some patients may need additional procedures in the future.
Can lifestyle changes alone treat this condition?
Lifestyle changes help but usually can't reverse significant artery narrowing.
What are the risks of these treatments?
Risks include bleeding, infection, and rarely, bowel injury; discuss with your doctor.
A Personalized Approach
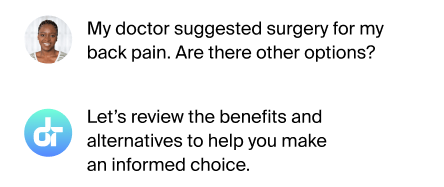
Treatment for chronic mesenteric ischemia should be tailored to each patient's specific situation, considering factors like overall health, extent of disease, and personal preferences.
Additional References
- Oderich GS, Tallarita T, Gloviczki P, et al. Mesenteric artery complications during angioplasty and stent placement for atherosclerotic chronic mesenteric ischemia. J Vasc Surg 2012; 55:1063.
- Lejay A, Georg Y, Tartaglia E, et al. Chronic mesenteric ischemia: 20 year experience of open surgical treatment. Eur J Vasc Endovasc Surg 2015; 49:587.
- Björck M, Koelemay M, Acosta S, et al. Editor's Choice - Management of the Diseases of Mesenteric Arteries and Veins: Clinical Practice Guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017; 53:460.
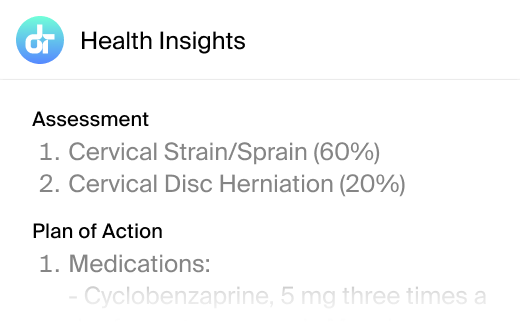
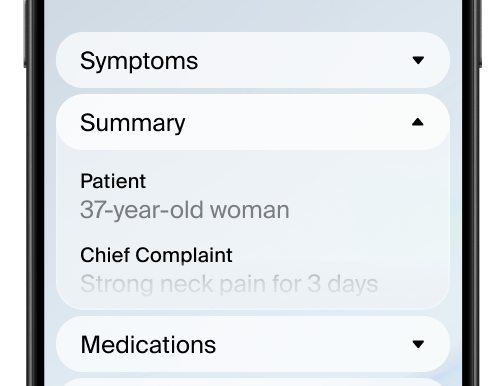
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.