Contents
-
Non-Pharmacological Approaches
-
Medication Options
-
Cardiac Interventions
-
Treating Underlying Conditions
Treating Syncope: From Simple Fixes to Advanced Interventions
Treating Syncope: From Simple Fixes to Advanced Interventions
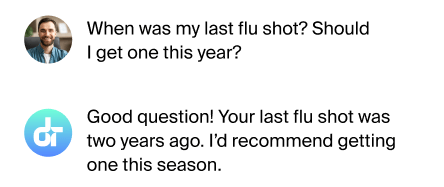
Tailored Treatments
Treating syncope effectively requires a personalized approach based on the underlying cause. From lifestyle changes to medical interventions, various strategies can help manage and prevent fainting episodes.
Contents
-
Non-Pharmacological Approaches
-
Medication Options
-
Cardiac Interventions
-
Treating Underlying Conditions
Non-Pharmacological Approaches
For many people with syncope, non-drug treatments are the first line of defense. These may include lifestyle modifications like increasing fluid and salt intake, avoiding triggers, and learning counter-pressure maneuvers. Physical counterpressure maneuvers, such as leg crossing or hand gripping, can help maintain blood pressure. Some patients benefit from tilt training, which involves gradually increasing tolerance to standing.
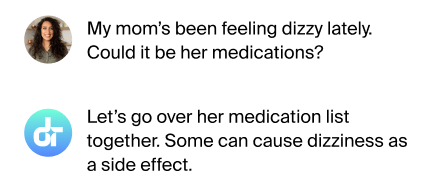
Medication Options
When lifestyle changes aren't enough, medications may be prescribed. For vasovagal syncope, drugs like fludrocortisone or midodrine might be used to boost blood volume or constrict blood vessels. Beta-blockers can help in certain cases of cardiac syncope. It's crucial to work closely with your doctor to find the right medication and dosage, as these drugs can have side effects.
Cardiac Interventions
For syncope caused by heart rhythm problems, cardiac interventions may be necessary. This could involve implanting a pacemaker to regulate heart rate in cases of bradycardia. For some arrhythmias, catheter ablation procedures can correct the heart's electrical pathways. In rare cases of severe cardiogenic syncope, an implantable cardioverter-defibrillator (ICD) might be recommended.
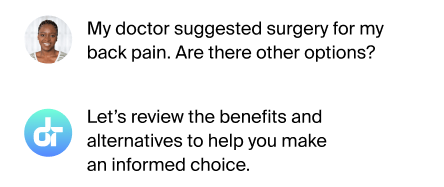
Treating Underlying Conditions
Sometimes, syncope is a symptom of another medical condition. Treating the underlying issue is key to managing syncope in these cases. This could involve managing diabetes to prevent blood sugar fluctuations, treating anemia to improve oxygen delivery, or addressing neurological conditions that affect blood pressure regulation. A comprehensive approach often yields the best results.
FAQs
How long does syncope treatment take?
Treatment duration varies based on the cause and chosen approach.
Can syncope be cured completely?
Many cases can be effectively managed, but some may require ongoing treatment.
Are syncope treatments covered by insurance?
Most treatments are covered, but check with your provider for specifics.
Can alternative therapies help with syncope?
Some find benefit, but discuss with your doctor first.
Is surgery ever needed for syncope?
Rarely, for specific cardiac causes or to implant devices.
A Path Forward
With the right treatment approach, most people with syncope can significantly reduce or eliminate fainting episodes and improve their quality of life.
Additional References
-
Brignole M, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 2018; 39:1883.
-
Shen WK, et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope. J Am Coll Cardiol 2017.
-
Solbiati M, et al. Implantable loop recorder versus conventional diagnostic workup for unexplained recurrent syncope. Cochrane Database Syst Rev 2016; 4:CD011637.
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.