Treating Unilateral Renal Artery Stenosis: Medical Therapy vs. Revascularization
Treating Unilateral Renal Artery Stenosis: Medical Therapy vs. Revascularization
The Treatment Dilemma
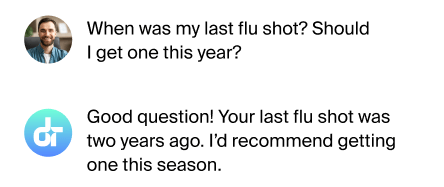
When it comes to treating unilateral renal artery stenosis, doctors face a challenging decision: should they use medications alone or combine them with a procedure to open the narrowed artery? This choice can have significant impacts on a patient's blood pressure and kidney function.
Contents
- Medical Therapy: The First Line of Defense
- Revascularization: Opening the Artery
- Weighing the Options
Medical Therapy: The First Line of Defense
Medical therapy is the cornerstone of treatment for unilateral renal artery stenosis. Doctors typically prescribe medications to control blood pressure and reduce the risk of complications. ACE inhibitors and ARBs are often the drugs of choice, as they can effectively lower blood pressure and protect kidney function. Other medications may include diuretics, calcium channel blockers, or beta-blockers, depending on the patient's specific needs.
Revascularization: Opening the Artery
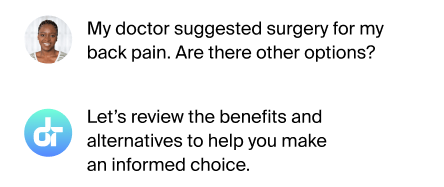
Revascularization procedures aim to physically open the narrowed renal artery. The most common method is percutaneous transluminal renal angioplasty (PTRA), often combined with stenting. During this procedure, a small balloon is inflated inside the artery to widen it, and a stent may be placed to keep it open. Surgical options, such as bypass grafting, are less common but may be necessary in complex cases.

Weighing the Options
The decision between medical therapy alone and revascularization is not always clear-cut. Recent studies have shown that for many patients, medical therapy can be just as effective as revascularization in controlling blood pressure and preserving kidney function. However, certain patients may benefit more from revascularization, such as those with recent onset of high blood pressure, uncontrolled hypertension despite multiple medications, or recurrent flash pulmonary edema.
FAQs
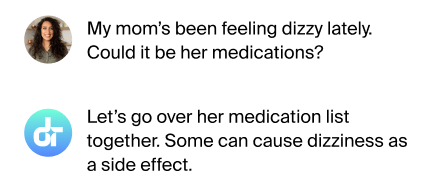
Is revascularization always better than medication?
Not always; effectiveness depends on individual patient factors.
Are there risks to revascularization procedures?
Yes, including potential complications like bleeding or artery damage.
How long does it take to see results from treatment?
It can vary, but improvements may be seen within weeks to months.
Can lifestyle changes help alongside medical treatment?
Yes, healthy diet and exercise can support overall treatment effectiveness.
Making the Right Choice
The best treatment approach for unilateral renal artery stenosis depends on each patient's unique situation and should be decided through careful consultation with healthcare providers.
Additional References
- Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med 2014; 370:13.
- ASTRAL Investigators, Wheatley K, Ives N, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953.
- Dworkin LD, Cooper CJ. Clinical practice. Renal-artery stenosis. N Engl J Med 2009; 361:1972.
This article has been reviewed for accuracy by one of the licensed medical doctors working for Doctronic.